Health and Global Policy Institute (HGPI) has published the discussion points “Considering Comprehensive Genomic Profiling from the Perspective of Patient Access: Utilizing the Medical Service Fee Reimbursement System and the Mixed Medical Services Program to Meet the Needs of Today.”
Since comprehensive genomic profiling (CGP) was granted insurance coverage in 2019, people serving in clinical settings have built experience with genomic cancer medicine, and findings from various studies continue to accumulate. In June 2023, Japan enacted the “Act on the Comprehensive and Systematic Promotion of Policies to Ensure that the Public Can Receive High-Quality and Appropriate Genome Medicine with Peace of Mind” or the Genome Medicine Promotion Act, and momentum for the promotion of genomic cancer medicine continues to grow. However, various issues must be addressed before appropriate genomic cancer medicine can be broadly provided to patients.
On June 11, 2025, a joint report titled “Briefing Report on Solid Cancer Treatment Based on Gene Panel Testing Using Next-Generation Sequencers” was presented by the Japanese Society of Medical Oncology (JSMO), the Japanese Cancer Association (JCA), and the Japan Society of Clinical Oncology (JSCO). Guidance provided by these three societies was utilized as an important foundation when CGP was granted insurance coverage in 2019, and the 2025 Briefing Report is another resource that should be used as guidance during the next revision of the medical service fee schedule. Now is precisely the time that it is critical for us to deepen discussions and take concrete action to promote genomic cancer medicine so its benefits can be delivered to patients in a more appropriate manner.
In light of this, HGPI hosted a policy dialogue convening stakeholders from industry, government, academia, and civil society to exchange views on the current landscape, ongoing challenges, and future directions of cancer genomic medicine in Japan.
This discussion points document outlines the concrete actions and future directions that stakeholders across industry, government, academia, and civil society must pursue to ensure that cancer genomic medicine truly translates into tangible benefits for patients.
For details, please see the PDF at the bottom.

On October 29, 2025, Health and Global Policy Institute (HGPI) and the Planetary Health Alliance Japan Hub co-hosted an open session titled “Municipalities × Planetary Health × Public Health” at the 84th Annual Meeting of the Japanese Society of Public Health.
The session brought together participants from a diverse range of positions, including mayors, researchers, practitioners, and students to explore how concrete local issues – such as elder care, living environments, and community-based healthcare coordination – can be addressed through the lens of Planetary Health, which recognizes the “interdependence of human health and the health of the Earth’s natural systems”. Participants discussed practical action plans to generate co-benefits for both health and the environment.
[Overview]
- Date & Time: Wednesday, October 29, 2025, 14:50-16:20 JST
- Format: In-person (Group Work)
- Venue: Room 910, 9th Floor, Venue 8, Granship Shizuoka Convention & Arts Center
- Language: Japanese
- Co-hosts: Health and Global Policy Institute (HGPI), Planetary Health Alliance Japan Hub
Introduction: Towards Action Plans Rooted in Local Challenges
The session opened with introductory remarks from Co-Chairs Prof. Saori Kashima (Director, Planetary Health Innovation Science Center, IDEC Institute for Peace and Coexistence, Hiroshima University / Associate Professor, Laboratory of Environmental Health Sciences, Graduate School of Advanced Science and Engineering, Hiroshima University / Steering Committee Member, Planetary Health Alliance Japan Hub) and Mr. Shu Suzuki (Senior Associate, HGPI).
They explained that the objective of the session was to consider how Planetary Health perspectives can be incorporated into local action plans to address issues related to elderly health, living environments, and healthcare service delivery. They both shared the concept of “human health and the global environment being mutually dependent,” which is at the core of Planetary Health, and they highlighted the importance of multisectoral collaboration among municipalities, public health centers, local communities, and research institutions.
Keynote Explanation: What is Planetary Health?
Prof. Chiho Watanabe (Professor, Graduate School of Tropical Medicine and Global Health, Nagasaki University / Chair, Planetary Health Alliance Japan Hub) delivered a keynote presentation titled “What is Planetary Health?”
Professor Watanabe described the essence of Planetary Health as the idea that “a better society can only exist on a healthy environment,” stressing that human development and environmental conservation must advance simultaneously. Referring to the Millennium Ecosystem Assessment, he explained that while humanity has enjoyed increased longevity and economic growth since the second half of the 20th century, the overexploitation of natural resources have simultaneously driven three major crises – climate change, biodiversity loss, and environmental pollution – all of which ultimately threaten human health and well-being.
He also introduced the concept of planetary boundaries, noting that several boundaries are already in a critical state. In this context, he argued that previous implementation of the SDGs has tended to sideline nature-related goals and emphasized the need to understand economic, social, and environmental goals as an “integrated wedding cake structure”.
Planetary Health, he concluded, is a new framework that focuses on the interactions between these elements and calls for pursuing human wellbeing within the limits of the Earth’s systems, with a long-term perspective that includes future generations.
 |
 |
Case Presentation (1): The Healthy City Approach
Prof. Keiko Nakamura (Professor Emerita, Institute of Science Tokyo /Director, Authorized NPO Healthy City Support Organization / Steering Committee Member, Planetary Health Alliance Japan Hub) presented the “Healthy City” approach as a practical entry point for implementing Planetary Health at the local level.
A Healthy City is defined as a city that aims to improve the well-being of its residents by integrating health considerations across sectors – including not only healthcare but also the natural environment, economic activities, urban infrastructure, and communities. Professor Nakamura outlined eight key elements for realizing this vision, placing particular emphasis on:
- Incorporating health perspectives into all policies (Health in All Policies)
- Establishing cross-sector collaboration among government departments, citizens, companies, and civil society organizations
- Ensuring leadership, good governance, and institutionalization of initiatives to sustain efforts over time
These elements were presented as important guiding principles for municipalities seeking to implement the concept of Planetary Health into concrete policies.
Case Presentation (2): Fukuroi City, Shizuoka Prefecture “From Local to Global – Practices in Food, Health, and Sustainability”
From Fukuroi City, Mr. Noriyuki Oba (Mayor) and Mr. Koji Ishizuka (Municipal Official) introduced the city’s long-term efforts. Fukuroi, a city of approximately 87,000 residents, declared itself “Japan’s Leading Healthy Cultural City” about 30 years ago. Through codifying this vision into an ordinance, the city has been linking health promotion with urban development from an early stage.
Mayor Oba explained that the city prioritizes not only “mental and physical health,” but also the “health of the city and nature,” and has incorporated lessons from international Healthy City networks into its policies.
Mr. Ishizuka presented concrete measures based on the “Fukuroi City Health Promotion Plan,” which aims to make Fukuroi “the city with the longest healthy life expectancy in Japan.” Key initiatives include addressing issues such as increasing risks of diabetes and hypertension, as well as the increasing incidence of skipping breakfast and rising obesity among children.
Particular attention was given to food-related initiatives directly connected to Planetary Health:
- Use of Local Produce and Food Education: Incorporating locally produced ingredients in school meals to make children learn about the journey of food from production to consumption.
- Co-benefits of Salt Reduction and Food Loss Reduction: By improving the taste and appeal of school meals and reducing salt content, Fukuroi is promoting the prevention of non-communicable diseases while reducing plate waste simultaneously.
- CO₂ Reduction: Using local produce reduces food miles. Research has shown an annual reduction of 15.37 tons of CO₂ emissions, demonstrating the environmental benefits of these efforts.
In addition, Fukuroi supports corporate health management by combining tools such as vegetable intake measurement (Veggie Check), data analysis using AI, and exercise programs to simultaneously improve employee health and corporate sustainability.
This case was shared as a noteworthy example of a Planetary Health initiative that uses local school meals and food education to realize a state in which “both people and the environment are healthy.”
Case Presentation (3): Kameyama City, Mie Prefecture “Green Healthy City and Biodiversity Conservation”
Mr. Yoshiyuki Sakurai (Mayor, Kameyama City) introduced Kameyama, a city of about 50,000 residents with a history as a post town and a strong manufacturing base. Under the vision of “Green Healthy City, Kameyama,” the municipality is promoting urban development that enhances residents’ quality of life (QOL) while conserving the natural environment.
Mayor Sakurai emphasized the importance of integrating health, culture, and community perspectives into urban, economic, and industrial policies, and highlighted the city’s efforts to address global biodiversity loss at the local level through:
- Introduction of a Regional OECM System: To contribute to the global “30 by 30” target, Kameyama designated conservation areas managed by citizens and companies as Other Effective area-based Conservation Measures (OECM), establishing a framework in which the municipality leads biodiversity conservation.
- Nature Positive Declaration and Water Source Forest Conservation: The city promotes reforestation in the headwaters of the Suzuka River under local ordinances, aiming to secure safe drinking water while preserving forest ecosystems.
- Nature Restoration and Health Promotion: Collaborations with citizen groups to restore natural environments and maintain satoyama and mountain trails provide opportunities for physical activity, contact with nature, and improved mental wellbeing.
These initiatives were presented as an example of “Planetary Health-oriented urban management”, which simultaneously advances nature conservation, citizen health, and resilience to disasters.
 |
 |
Group Work: First Steps for “Municipalities × Planetary Health”
Following the presentations, participants divided into six groups to discuss feasible action plans in their own contexts, using the idea of co-benefits – measures that are “good for both the environment and health” – as a guiding principle. Key points from each group included:
- Group A: Existing Initiatives and Organizational Silos
Participants shared examples of ongoing initiatives related to Planetary Health, such as food education and nature co-existence programs. However, departmental silos were identified as a major barrier to collaboration among health, construction, transportation, and other sectors. The group emphasized the need to establish cross-departmental teams or coordinating mechanisms.
- Group B: Co-benefit Actions and Multisectoral Collaboration
Proposals included “zero food loss” efforts, “plogging” (jogging while collecting litter), and the use of green curtains as a heat countermeasure that also promotes outdoor activity. To scale such efforts, the group suggested forming core teams across sectors, strengthening shared understanding among staff, and encouraging family-based participation as a sustainable approach.
- Group C: Low-cost Approaches to Align Environment and Health
Participants discussed practical, low-cost options such as reducing food loss, promoting local produce, using existing facilities (e.g., shopping centers) as spaces for physical activity, and reducing single-use materials in healthcare settings. They also underlined the need to address environmental and social inequities, particularly in heat countermeasures for vulnerable populations.
- Group D: Aso Grasslands Conservation and Cross-sectoral Benefits
Using the case of the Aso grasslands as an example, the group examined how protecting a single local resource can connect education, public health, tourism, and the economy. They concluded that grassland conservation can generate multiple benefits when various sectors collaborate, including disease prevention, disaster risk reduction, and regional revitalization.
- Group E: Connecting Individual Choices and Organizational Strategies
This group focused on the importance of individual awareness and behavior change while recognizing the challenges of scaling such changes across communities. Proposals included clarifying contact points within governments and companies for Planetary Health-related initiatives and conducting “internal analyses” of each organization’s mandate and resources to identify realistic pathways for collaboration.
- Group F: Island Communities, Tradition, and Environmental Change
Drawing on experiences from remote islands in Okinawa, participants discussed how traditional lifestyles, diets, and fishing practices are closely connected to both health and the environment. While initiatives such as “catch and eat local fish” contribute to physical activity and lower environmental impact, concerns were raised about the potential impacts of climate change on marine ecosystems and the sustainability of such practices.
Across all groups, there was shared recognition that reframing existing initiatives and local resources through a Planetary Health lens and fostering collaboration across sectors constitute practical first steps for municipalities.
 |
 |
Conclusion and Next Steps
In conclusion, Professor Watanabe commended participants for articulating concrete ideas and Planetary Health perspectives within a limited timeframe, emphasizing that progress in public–private collaboration depends on each individual taking initiative to build teams and drive change within their own context.
Dr. Kashima noted that the issues raised in this 90-minute session were wide-ranging and could not be fully explored within the available time. He highlighted that the Planetary Health Alliance is planning to hold its Annual Meeting in Tokyo in 2027, and expressed hope that the discussions and practices emerging from Japan’s municipalities will help shape contributions to that global platform.
Building on this session, HGPI will continue to work with municipalities, research institutions, and civil society to advance public health policy from a Planetary Health perspective and to provide spaces for dialogue among diverse stakeholders.
[Speaker Profiles]
Chiho Watanabe (Professor, School of Tropical Medicine and Global Health, Nagasaki University)
Chiho Watanabe withdrew from the doctoral program at the Graduate School of Medicine, The University of Tokyo in 1989 after completing required coursework. He was appointed Professor of Human Ecology at the same graduate school in 2005. In 2017, he became President of the National Institute for Environmental Studies (NIES), a national research and development agency. From 2021 to 2022, he served as Professor and Special Advisor to the President (Planetary Health), School of Tropical Medicine and Global Health, Nagasaki University. From 2022 to 2023, he served as the first Dean of the Interfaculty Initiative in Planetary Health and continued as Professor at the same school. He is currently Professor Emeritus at the University of Tokyo and holds a Doctorate in Health Science. His previous roles include President of the Japanese Society of Health and Human Ecology (2017–2022), President of the Society of Environmental Science, Japan (2021–2023), Associate Member of Section II of the Science Council of Japan, former Third Vice President of the Society for Human Ecology, and former Chair of the Human Ecology Section of the Ecological Society of America. He currently serves as a Steering Committee Member of the Planetary Health Alliance (PHA) and Representative of the Planetary Health Alliance Japan Hub.
Keiko Nakamura (Professor Emeritus, Institute of Science Tokyo)
Keiko Nakamura graduated from the Faculty of Medicine at Tokyo Medical and Dental University. She served as Professor in the Department of Global Health Entrepreneurship at the Graduate School of Medical and Dental Sciences at the same university from 2016 to 2025, and became Professor Emeritus at the Institute of Science Tokyo in April 2025. Her past appointments include Board Member of the Society of Environmental Science, Japan (2013–2017), Director of the WHO Collaborating Centre for Healthy Cities and Urban Policy Research (2016–2024), Board Member of the Japanese Society of Public Health (since 2017), Member of the Urban Health and Wellbeing Scientific Committee of the International Science Council (since 2020), and Chair of the Environmental Risk Subcommittee, Science Council of Japan (since 2024). Her research focuses on urban environment and health, health promotion, and Planetary Health.
Noriyuki Oba (Mayor of Fukuroi City, Shizuoka Prefecture)
Born in 1963 in Ugari (Dainichi), Fukuroi City, Shizuoka Prefecture, Noriyuki Oba graduated from the Faculty of Science and Technology at Keio University in 1987 and joined HORIBA, Ltd. the same year. From 1988 to 1992, he was stationed at Horiba Europe in France. In 1993, he became a Director at Wada Juku Co., Ltd., and in 1994, a Director at Showa Co., Ltd. He was first elected to the Shizuoka Prefectural Assembly in 2001 and became a Director of Scene Making Co., Ltd. in 2003. In 2009, he was appointed President and CEO of Wada Juku (now Lighthouse Education Co., Ltd.) and also assumed the role of Representative of ISC Ryugaku-net, a study abroad support service. He became Chairman of the Board in 2015 and Honorary Chairman in 2021. In April 2021, he was elected Mayor of Fukuroi City and is currently serving his first term.
Yoshiyuki Sakurai (Mayor of Kameyama City, Mie Prefecture)
Born in Mie Prefecture in 1963, Yoshiyuki Sakurai graduated from Mie Prefectural Kobe High School in 1981 and from the Faculty of Sociology at Kansai University in 1986. He began his political career as a member of the Kameyama City Council in 1991 (serving one term) and went on to serve four consecutive terms in the Mie Prefectural Assembly from 1995 to 2008. During his time in the prefectural assembly, he held key positions including Chair of the Council for the Promotion of Linear Construction, Mie Prefectural Auditor, and the 101st Vice Speaker of the Assembly. In 2009, he was elected Mayor of Kameyama City and is now serving his fifth consecutive term as of 2025. As mayor, he has worked to strengthen inter-municipal collaboration in Mie Prefecture, serving as Vice President (2015–2016), President (2019–2020), and Auditor (2023–2024) of the Mie Prefecture Mayors Association. He currently serves in multiple leadership roles, including: Head of the Japanese Chapter of the Alliance for Healthy Cities, Board Member of the National Council for the Preservation of Historic Districts for Traditional Buildings, Director of the Mie Prefecture Civil Infrastructure Development Association, and Vice Chair of the Suzuka-Kameyama Regional Union. His motto is: “Think big, start small.”
■ Health and Global Policy Institute (HGPI) https://hgpi.org/en/
Health and Global Policy Institute (HGPI) is a non-profit, independent, non-partisan health policy think tank established in 2004. In its capacity as a neutral think-tank, HGPI involves stakeholders from wide-ranging fields of expertise to provide policy options to the public to successfully create citizen-focused healthcare policies. Looking to the future, HGPI produces novel ideas and values from a standpoint that offers a wide perspective. It aims to realize a healthy and fair society while holding fast to its independence to avoid being bound to the specific interests of political parties and other organizations. HGPI intends for its policy options to be effective not only in Japan, but also in the wider world, and in this vein the institute will continue to be very active in creating policies for resolving global health challenges.
■ Planetary Health Alliance Japan Hub https://phajapan.jp/english
The concept of Planetary Health was introduced in the 2015 report “Safeguarding Human Health in the Anthropocene Epoch,” published by the Rockefeller Foundation–Lancet Commission on Planetary Health in The Lancet in 2016. In the same year, key members of the commission established the Planetary Health Alliance (PHA), a consortium now based at Johns Hopkins University in the United States. PHA has since become a global network of more than 400 universities, NGOs, research institutes, and government agencies from over 60 countries, serving as a leading force in the rapid growth of this interdisciplinary field. In May 2023, the Planetary Health Alliance Japan Hub was established with its secretariat hosted by Nagasaki University. The Japan Hub has since been facilitating discussions to explore frameworks for Planetary Health tailored to Japan and the broader Asia-Pacific region, where the relationship between nature and human society is uniquely situated. The Hub welcomes participation from a wide range of disciplines and age groups—from students to senior professionals.
Health and Global Policy Institute (HGPI) has submitted public comments on the Ministry of the Environment’s published “Interim Evaluation of the Implementation Status of the National Biodiversity Strategy 2023-2030 (Draft)” and the “7th National Report under the Convention on Biological Diversity (Draft)”.
The “Interim Evaluation of the Implementation Status of the National Biodiversity Strategy 2023-2030 (Draft)” is being conducted in accordance with the Basic Act on Biodiversity. This evaluation is required by the Basic Act on Biodiversity and follows the strategy that the Cabinet approved in March 2023. The strategy requires regular progress checks on its goals and actions, including interim and final evaluations that align with international reporting deadlines for the Global Review.
Furthermore, the “7th National Report under the Convention on Biological Diversity (Draft)” is being prepared because Article 26 of the Convention on Biological Diversity requires each Party to submit a national report summarizing the status of implementation of the Convention to the Conference of the Parties.
Biodiversity is the foundation supporting health of ecosystem and is closely linked to planetary health and One Health approach. Against this backdrop, our organization proposed the following perspectives:
- Regarding the impact of microplastics, consider not only biological ecosystems but also risks to human health.
- When promoting Nature-based Solutions (NbS), it is essential to raise awareness of the importance of scientifically evaluating their co-benefits for human health.
- Position health damage to local communities caused by the degradation of natural capital as a new critical issue in health management.
- Capture changes in demand driven by increased public interest in mental health and well-being, as it relates to the types of use and services required in national parks, quasi-national parks, and national monuments.
- Explicitly state the One Health perspective, which integrates biodiversity conservation and public health.
Our organization will continue to contribute to advancing planetary health through policy proposals and collaboration with relevant organizations, by providing insights and promoting dialogue.

Health and Global Policy Institute (HGPI) hosted an installment of 30-minute Health Policy Update, which is held on an irregular basis to brief non-partisan Diet members on key health policy issues. The concept of this installment was “Considering the Future of Health and Medical Policy with Industry, Government, Academia, and Civil Society.” Working more closely with the legislature than ever before and with support from our non-partisan promoters, our objective was to deepen learning for non-partisan Diet members using concrete and verifiable data in themes with a high degree of public interest including cancer, preventive medicine, internal and surgical diseases, pediatrics, and perinatal care and, with a future-oriented vision, have an equal exchange of opinions on next steps.
[Program] (Titles omitted)
Lecture “The Best Investment is Prevention – Controlling Healthcare Costs and the Strategic Use of Colorectal Cancer Screening”
Masao Okubo (Deputy Director, Sanno Hospital; Specialist in Gastroenterology)
Takahisa Matsuda (Department of Gastroenterology, Division of Internal Medicine, Faculty of Medicine, Toho University)
Q&A and Discussion
■Non-partisan Diet Member promoters (titles omitted; in Japanese syllabary order)
Members of the House of Representatives:
Keishi Abe, Naoyuki Ito, Satoshi Umemura, Hiroaki Tabata, Katsuhito Nakajima, Mitsuko Numazaki, Toru Fukuda
Members of the House of Councillors:
Kozo Akino, Takahiro Anno, Katsuo Oshima, Akira Koike, Hiroyuki Konishi, Hanako Jimi, Mami Tamura, Toshiharu Furukawa

Chronic Obstructive Pulmonary Disease (COPD) is recognized as a disease with a substantial burden both domestically and internationally, and is considered to impose significant healthcare costs. While the risk factors for COPD are predominantly attributed to daily inhalation of harmful substances such as smoking and air pollution, a key characteristic of the disease is that clinical symptoms are often difficult to detect in its early stages. As a result, it is believed that there are many potential patients who remain undiagnosed or have not sought medical care despite being affected.
COPD presents challenges in achieving early detection and continuous treatment due to the limited availability of spirometry (pulmonary function testing) necessary for diagnosis, as well as the difficulty in recognizing gradually changing symptoms in daily life. Given these challenges, public understanding of COPD and other respiratory diseases, engagement in preventive behaviors, and awareness of the need for regular medical care remain insufficient. Meanwhile, delayed intervention for declining respiratory function can negatively affect overall health, including cardiac function, bone density, nutritional status, and mental health. Moreover, COPD frequently coexists with leading causes of mortality such as heart disease and lung cancer, acting as an exacerbating factor or hindering treatment. Therefore, deepening interest in and understanding of COPD also contributes to raising public awareness of respiratory symptoms and improving comprehension of respiratory diseases. In light of these connections, early detection of COPD is a critical public health issue closely linked to the urgent need for strengthened and expanded healthcare systems.
While efforts are underway to develop early detection methods that do not rely on effort-dependent pulmonary function tests required for diagnosis, challenges have also been identified in healthcare delivery systems and medical access, including an insufficient number of specialists relative to the estimated patient population. To advance these initiatives, support through legal and institutional frameworks remains inadequate compared to other medical fields, necessitating policy-level responses.
In this HGPI Seminar, we will focus on COPD, a disease with a high number of potential patients due to characteristics of Japan’s healthcare environment and lifestyle. We are honored to welcome Dr. Shigeo Muro from Nara Medical University, who will deliver a comprehensive lecture covering a broad range of topics—from healthcare-seeking behaviors expected of citizens and patients to policy challenges that should be addressed at the municipal and national levels.
Drawing on his extensive experience in both clinical practice and research, Dr. Muro will provide concrete insights into the role and potential of respiratory medicine within the healthcare system from both scientific and policy perspectives. Using COPD as a lens, we hope this seminar will serve as an opportunity to reaffirm the challenges and possibilities of the overall healthcare system and to inspire actions for improvement ranging from the individual to the policy level.
[Event Overview]
- Speaker:
Dr. Shigeo Muro (Professor, Department of Respiratory Medicine, Nara Medical University / Vice Director, Nara Medical University Hospital) - Date & Time: Tuesday, January 27, 2026, 18:00-19:15 JST
- Format: Online (Zoom webinar)
- Language: Japanese
- Participation Fee: Free
- Capacity: 500 participants
■Profile:
Dr. Shigeo Muro (Professor, Department of Respiratory Medicine, Nara Medical University / Vice Director, Nara Medical University Hospital)
Professor Muro graduated from Kyoto University Faculty of Medicine in 1989 and worked at Tazuke Kofukai Kitano Hospital before completing his doctoral program at Kyoto University Graduate School in 1998 (Ph.D. in Medicine). After serving as a research fellow at McGill University Meakins-Christie Laboratories and as lecturer and associate professor at Kyoto University, he assumed his current position in 2018. He serves as Executive Director and Chair of the Insurance Committee of the Japanese Respiratory Society. He served as Chief Editor and Vice-Chair for the 5th through 7th editions of the society’s ‘Guidelines for the Diagnosis and Treatment of COPD’ and as Chair for the 2nd edition of ‘Guidelines for the Diagnosis and Treatment of Asthma and COPD Overlap’ (published in 2024). He is also actively involved in ‘Komorebi 2032,’ the society’s project aimed at reducing COPD mortality rates. He received the 1st Prize of the 42nd Baelz Award (2005) and the Japanese Respiratory Society Kumagai Award (2014).

Health and Global Policy Institute (HGPI) will host an urgent symposium to examine the significance, rationale, and practical approaches for reflecting the voices of patients and people with lived experience in the Central Social Insurance Medical Council (CSIMC), as discussions on its reform accelerate.
On October 20, 2025, a new coalition government was formed by the Liberal Democratic Party and the Japan Innovation Party, placing social security reform as a top policy priority. Among these priorities, the proposed “reform of CSIMC” is a particularly important theme that is expected to have a substantial impact on future healthcare policy decision-making processes.
CSIMC is a key advisory council under the Ministry of Health, Labour and Welfare, with significant influence over revisions to medical service fees and drug prices. However, under the current system, no formal framework exists for “patient representatives,” and it is difficult to say that patient and public perspectives are sufficiently reflected in policy design.
Against this backdrop, this symposium will explore, in view of the direction of CSIMC reform under the new administration:
- The significance and legitimacy of patient and public involvement in CSIMC
- Effective ways to bring patients and public voices into the policy process
- The mechanisms and selection processes needed to ensure meaningful participation
In addition, HGPI will invite applications from individuals registered on the “Japan’s Patient Expert Platform (J-PEP)” to serve as panelists in the symposium’s panel discussion. (Detailed application information is available on the J-PEP members-only page after registration.)
■ For more information about J-PEP, please click here.
This will be HGPI’s first attempt to directly recruit panelists from among patients and people with lived experience, and we view this as an important opportunity to bring diverse voices into policy-making. We warmly welcome and encourage your active participation.
|
*The deadline for In-person participation is
Wednesday, January 14, 2026, at 23:59 |
*The application deadline is
Thursday, 18 December 2025 at 23:59 |
To participate in this seminar, J-PEP membership registration is required.
(Registration is free, but please note that J-PEP is available only in Japanese.)
[How to Register]
- If you are not yet a member, please register for J-PEP.
- After completing registration, please log in.
- Once logged in, please complete your seminar registration here.
(Available only in Japanese.)
[Event Overview]
- Date & Time: Thursday, January 22, 2026; 14:00-16:00 JST
- Format: In-person only (Please note that video of this event will not be streamed or archived)
- Venue: Conference Room 22A, TKP Tokyo Station Otemachi Conference Center (KDDI Otemachi Building 22F, 1-8-1 Chiyoda City, Tokyo)
- Language: Japanese only
- Participation Fee: Free
- Capacity: 50 participants
*First-come, first-served basis (Seats for media representatives who wish to cover the event will be arranged separately.)
[Program] (Titles omitted; speaker list and content is subject to change)
| 14:00-14:10 | Opening Remarks and Explanatory Introduction |
| Shunichiro Kurita (Senior Manager, HGPI) | |
| 14:10-14:45 | Short Lectures: “Discussion Points for CSIMC Reform” (5 minutes each) |
|
Naomi Sakurai (President, Cancer Survivors Recruiting Project) |
|
| 14:45-15:30 | Panel Discussion: “Necessary Actions for Delivering Patients’ Voices Through CSIMC” |
|
Panelists: |
|
| 15:30-15:55 | Question and Answer Session with the Audience |
| 15:55-16:00 | Closing Remarks |
| Ryoji Noritake (Chair, HGPI) |

Health and Global Policy Institute (HGPI) co-hosted a roundtable with UHC2030, the Asian Development Bank (ADB), the Civil Society Engagement Mechanism for UHC2030 (CSEM), and the Global Health Civil Society Network (GH-Net). The discussion focused on advancing Universal Health Coverage (UHC) in the Asia–Pacific region and Japan, particularly on strengthening financial risk protection to safeguard people from the economic hardship caused by out-of-pocket health expenditures.
Across the Asia–Pacific region, more than one billion people still lack access to essential health services, and out-of-pocket payments remain a major driver of impoverishment. In response to these challenges, ADB announced the establishment of a new peer-learning network, the Universal Health Coverage Practitioners and Experts Knowledge Exchange and Resources (UHC PEERS). This network is expected to work in close collaboration with the UHC Knowledge Hub in Tokyo, which was officially launched at the UHC High-Level Forum on December 6, to further support high-quality policy development.
Guided by this year’s International UHC Day theme, “Unaffordable health costs? We’re sick of it!”, the roundtable connected international trends with Japan’s domestic policy discussions. Participants engaged in a multifaceted dialogue on issues including the review of Japan’s High-Cost Medical Expense Benefit system and the importance of financial protection for vulnerable populations. Experts from Australia, the United Kingdom, the United States, the Philippines, Guinea-Bissau, and other countries contributed their perspectives, offering practical insights to advance UHC globally and within Japan.
This event not only facilitated the exchange of knowledge but also provided a valuable platform to advance domestic and international dialogue with civil society and a broad spectrum of stakeholders, building on the momentum of UHC Day and the UHC High-Level Forum.
 |
 |
[Event Overview]
- Date & Time: Friday, December 5, 2025, 14:30-16:30 JST
- Format: In-person
- Venue: Global Business Hub Tokyo, 3F, Otemachi Financial City Grand Cube, 1-9-2 Otemachi, Chiyoda-ku, Tokyo
- Language: English & Japanese (Simultaneous interpretation provided via Notta AI-assisted real-time transcription)
- Co-hosts:
– UHC2030
– Asian Development Bank (ADB)
– Health and Global Policy Institute (HGPI)
– Civil Society Engagement Mechanism for UHC2030 (CSEM)
– Global Health Civil Society Network (GH Network)
■ Speakers (title omitted, in no specific order)
Pamela Cipriano (Co-chair, UHC2030, Steering Committee)
Magda Robalo (Co-chair, UHC2030, Steering Committee)
Eduardo Banzon (Director for Health, Human and Social Development, ADB)
Akihito Watabe (Health Specialist, Human and Social Development, ADB)
Justin Koonin (President, ACON / Former UHC Political Advisor / Distinguished Fellow, The George Institute for Global Health)
Robert Yates (Visiting Professor in Practice, LSE Health)
Waiswa Nkwanga (Management Sciences for Health (MSH) / CSEM Secretariat)
Masaki Inaba (Co-Representative & Director of International Health Division, Africa Japan Forum (AJF) / Representative, Global Health Civil Society Network (GH Network) / Former CSEM Advisory Committee Member)
Akiko Mera (Executive Director, Médecins du Monde Japan / Global Health Civil Society Network (GH Network) / Former CSEM Advisory Committee Member)
Kyoko Ama (Founder, Children & Healthcare Initiative / Fellow, HGPI)
Junichi Kawata (Vice President, The Association of CML patients & families「IZUMI」/ Project Researcher, Public Policy Research, The Institute of Medical Science, The University of Tokyo)
Masanori Okuse (Representative Director, Japanese Association for Psoriatic Disease)
Satoshi Maemura (Senior Staff Writer, Nikkei Inc.)
Joji Sugawara (Vice President, HGPI / Advisory Committee Member, CSEM)

Health and Global Policy Institute (HGPI) held an Advisory Board meeting titled “Toward Reliable Policy Implementation for Early Detection and Early Intervention of Chronic Kidney Disease (CKD) at the Local Governments” on November 13, 2025.
In Fiscal Year 2024, HGPI conducted both quantitative and qualitative surveys to understand the reality of one of the major challenges in renal disease measures: the gap between health checkups and seeking medical care. Based on the findings of these surveys, discussions were deepened at an Advisory Board meeting, leading to the compilation of the policy recommendations document, “Policy Recommendations on Strengthening Chronic Kidney Disease Strategies: Challenges and Solutions in Seeking Medical Care from the Perspective of Patients and Those Affected”. The recommendations emphasized the importance of cross-sectoral discussions, the need to establish evidence-based standards for recommending medical visits, and the significance of prioritizing intervention groups and considering approaches tailored to specific attributes.
For Fiscal Year 2025, HGPI plans to hold two Advisory Board meetings. Building upon the previous year’s recommendations, the goal is to specifically clarify the challenges faced by local governments and health insurers in the CKD care pathwayーfrom health checkups to seeking medical careーand to organize and examine feasible solutions to these barriers, as well as the roles required of stakeholders to overcome them.
This first meeting focused on CKD countermeasures at the local governments. It was held to deepen discussions while sharing the current challenges with experts from various fields, aiming to identify concrete solutions that can be implemented by local governments.
*Based on the discussions from the first and second meetings, a set of policy recommendations will be developed and published.
[Event Overview]
- Date & Time: Thursday, November 13, 2025; 14:00-16:00 JST
- Format: Hybrid *This meeting was held as a closed session.
- Venue: Otemachi Financial City Conference Center (Otemachi Financial City South Tower, 1-9-7 Otemachi, Chiyoda-ku, Tokyo 100-0004)
- Language: Japanese
- Organizer: Health and Global Policy Institute (HGPI)
■Advisory board members (title omitted; in Japanese syllabary order)
Yayoi Kanameda (Deputy Director, Health Policy Group, Welfare and Health Division, Welfare and Health Department, Kure City)
Takeo Nakayama (Professor, Department of Health Informatics, School of Public Health, Kyoto University)
Satomi Baba (Deputy Director, Health Promotion Division, Public Health Center, Health and Welfare Department, Kurume City)
Akira Fukui (Lecturer, Division of Nephrology and Hypertension, Department of Internal Medicine, The Jikei University School of Medicine)
Shingo Fukuma (Professor, Department of Epidemiology, Infectious Disease Control and Prevention, Hiroshima University Graduate School of Biomedical and Health Sciences/ Professor, Human Health Sciences, Kyoto University Graduate School of Medicine)
Ayumi Matsumura (Section Chief, Cancer and Disease Control Section, Cancer and Disease Control Division, Regional Medical Department, Medical Bureau, Yokohama City)
Keiji Muramatsu (Project Professor, Center for Next Generation of Community Health, Chiba University Hospital)
Masaaki Yokota (Assistant Director-General, Health and Welfare Bureau, City of Chiba)
Moderator
Eri Yoshimura (Senior Manager, Health and Global Policy Institute)
The cross-sectional survey titled “Perceptions, Knowledge, Actions, and Perspectives on Climate Change and Health Among Healthcare Sector Organizations in Japan”, published on November 13, 2025, was featured in CB news. Additionally, it was featured in Forbes JAPAN on December 3.
This survey was conducted online to capture the perceptions, knowledge, actions, and policy views on climate change and health among academic societies, professional associations, and industry organizations in the Japanese healthcare sector. It was carried out ahead of the 30th Conference of the Parties (COP30) to the United Nations Framework Convention on Climate Change, scheduled for November 2025.
For the full survey report by our organization, please click here.
Please see the following articles (Japanese only):
- Forbes JAPAN
- CB news *Please note that visitors must register for a CBnews account.

Health and Global Policy Institute (HGPI) and AMR Alliance Japan Japan hosted an Open Meeting titled “AMR Measures as Regional Health Crisis Management: The Role of Public Health Professionals and Multidisciplinary Collaboration” at the 84th Annual Meeting of Japanese Society of Public Health on Thursday, October 30, 2025.
Antimicrobial resistance (AMR) is an urgent global and public health challenge, as explicitly stated in the World Health Organization (WHO)’s “Global Action Plan on AMR” and the Japanese government’s “National Action Plan on AMR (2023-2027)”. AMR not only complicates the treatment of infectious diseases in healthcare settings but also profoundly impacts the health management of local community as well as future healthcare delivery systems. Inappropriate antibiotic use accelerates the emergence of AMR, putting even specialized medical treatments like surgery and cancer therapy at risk.
Grounded in the overall theme of the conference, “Phase-Free Community Development and Health Crisis Management,” this session positioned AMR measures within routine public health activities, educational support for local residents, and awareness campaigns. It aimed to establish AMR measures as an integral part of everyday health crisis management in daily life.
In Shizuoka Prefecture, where the Annual Meeting was held, a multilayered, community-based AMR measures program is being developed. Through the Antibiotic Awareness, Shizuoka (AAS) team, which is a group of multidisciplinary volunteers, and the prefecture’s AMR subcommittee. The team collaborates with administrative bodies (the prefecture and public health centers), the clinical sector (medical institutions), the pharmacy sector (hospital pharmacy departments and pharmacists’ associations), medical associations, laboratory services (clinical and public health laboratories), and veterinary associations. They are advancing cross-sectoral initiatives that include supporting clinical practice, raising public awareness and aiding education, and fostering human resource development. This combination of bottom-up activity and collaboration between the administrative and medical sectors serves as an excellent practical model that can be a valuable reference for other regions. In this context, the Open Meeting provided an opportunity to reconsider municipal AMR measures from the perspective of “phase-free” health crisis management.
HGPI also held a preliminary Public Health Seminar in July 2025 targeting public health professionals and other professionals from local governments. Under the title “AMR Measures to Protect Community Health – A Public Health Perspective,” the seminar featured presentations from multiple local government and public health center representatives sharing concrete examples of municipal AMR initiatives. These practical examples highlighted the importance of integrating AMR measures into existing programs such as maternal and child health, food sanitation, and tuberculosis control for effective AMR management. Building on the discussions from the July seminar, the Meeting at the Annual Meeting of Japanese Society of Public Health provided a venue to examine AMR measures by local governments from both a broad policy perspective and a practical, on-the-ground standpoint.
The session opened with a presentation by Dr. Michiko Nagamine, Director of the Itabashi City Public Health Center in Tokyo, on the roles expected of local government staff in advancing AMR measures. This was followed by a presentation of a research report from HGPI on the current status and challenges of implementing AMR measures in local governments across Japan, which organized key issues from multiple angles.
In the latter half of the session, four panelists from diverse professional backgrounds joined a panel discussion. Shedding light on the “One Health Approach,” an integrated view of human, animal, and environmental health, they exchanged views on how to design phase-free AMR measures tailored to the specific characteristics of their own regions and work. The discussion also brainstormed concrete ideas on how to incorporate elements of AMR measures into person-to-person and object-oriented services such as daily health consultations, medical examinations, vaccinations, hygiene management, and food inspections, while linking them with specific project plans and action plans.
Through this Open Meeting, participants reaffirmed the critical role of public health professionals as hubs in cross-sectoral regional networks that connect government, clinical care, pharmacy, veterinary medicine, and other sectors, thereby strengthening community health crisis management capacity in both normal times and emergencies. Going forward, HGPI and AMR Alliance Japan will continue working with local governments and related organizations to advance practical, community-based AMR measures.
 |
 |
 |
 |
 |
 |
 |
 |

[Event Overview]
- Date & Time: Thursday, October 30, 2025, 18:00-20:00 JST
- Format: In-person
- Venue: Shizuoka Convention Arts Center “GRANSHIP”
2nd Floor Waiting Rooms 2 & 3 (the 84th Annual Meeting of the Japan Society of Public Health, Venue 15) - Language: Japanese
- Participation Fee: Free
- Capacity: 50 participants
- Organizers: Health and Global Policy Institute (HGPI), AMR Alliance Japan
[Program] (Titles omitted)
18:00-18:10 Opening Remarks and Introduction
Yui Kohno (Manager, HGPI / AMR Alliance Japan)
18:10-18:40 Presentation: AMR Countermeasures as Health Crisis Management: The Expected Role of Local Government Staff
Michiko Nagamine (Director, Itabashi City Public Health Center, Tokyo)
18:40-18:55 Research Report: Current Status and Challenges of AMR Countermeasures in Local Governments
Daichi Watanabe (Senior Associate, HGPI / AMR Alliance Japan)
19:00-19:55 Discussion: Considering Phase-Free AMR Countermeasures for My Region/Work
Panelists:
Kazutoshi Sugiyama (President, Shizuoka Veterinary Medical Association)
Toshihiro Tanaka (Chief of Pediatrics, Shizuoka Kosei Hospital)*
Michiko Nagamine (Director, Itabashi City Public Health Center, Tokyo)
Takahiro Mochizuki (Department of Pharmacy, Shizuoka Cancer Center)*
* Short presentations were delivered at the beginning of the session.
Moderator:
Yui Kohno (Manager, HGPI)
19:55-20:00 Summary and Closing Remarks
■ Speaker’s Profile (Titles Omitted)
Michiko Nagamine(Director, Itabashi City Public Health Center, Tokyo)
 Michiko Nagamine graduated from Tokai University School of Medicine. She had a strong interest in international health and tropical medicine since her medical school days, and studied abroad at the University of London and University of Nairobi, where she did clinical practice for about 9 months on a credit-exchange program. After graduation, she did her initial training in the Department of General Medicine at Kawasaki City Kawasaki Hospital. She then obtained a Diploma in Tropical Medicine (DTMH) at Mahidol University (Thailand), and worked as a researcher at the Kenya Medical Research Institute. Since 2003, she has worked as a public health physician for the Tokyo Metropolitan Government, serving in various municipalities including Shinjuku City, Setagaya City, and Minato City, engaging in infectious disease control, health promotion, and various activities. She has been in her current position since 2025. She is also an advisor to the Japanese Society of Tuberculosis, an advisor to the Japanese Society of Social Medicine, and is a certified specialist of the Japanese Society of Public Health, a certified internist of the Japanese Society of Internal Medicine, and a Doctor of Medicine.
Michiko Nagamine graduated from Tokai University School of Medicine. She had a strong interest in international health and tropical medicine since her medical school days, and studied abroad at the University of London and University of Nairobi, where she did clinical practice for about 9 months on a credit-exchange program. After graduation, she did her initial training in the Department of General Medicine at Kawasaki City Kawasaki Hospital. She then obtained a Diploma in Tropical Medicine (DTMH) at Mahidol University (Thailand), and worked as a researcher at the Kenya Medical Research Institute. Since 2003, she has worked as a public health physician for the Tokyo Metropolitan Government, serving in various municipalities including Shinjuku City, Setagaya City, and Minato City, engaging in infectious disease control, health promotion, and various activities. She has been in her current position since 2025. She is also an advisor to the Japanese Society of Tuberculosis, an advisor to the Japanese Society of Social Medicine, and is a certified specialist of the Japanese Society of Public Health, a certified internist of the Japanese Society of Internal Medicine, and a Doctor of Medicine.
Kazutoshi Sugiyama (President, Shizuoka Veterinary Medical Association)
 Dr. Sugiyama graduated from Azabu University’s School of Veterinary Medicine and later completed his Ph.D. there. His career includes roles at the Shizuoka Prefectural Poultry Experiment Station and Small Livestock Experiment Station (1984-1991), the Faculty of Agriculture at Shizuoka University (1987-1988), and as Representative Director of the Shizuoka City Emergency Animal Hospital (2015-2020). He currently serves the Director of the Sugiyama Veterinary Clinic, and holds numerous parallel posts, including committee member for the Japan Veterinary Medical Association, Vice President of the Shizuoka Animal Welfare Association, Vice President of the Japanese Clinical Society of Rabies, as well as a cooperative researcher at Azabu University.
Dr. Sugiyama graduated from Azabu University’s School of Veterinary Medicine and later completed his Ph.D. there. His career includes roles at the Shizuoka Prefectural Poultry Experiment Station and Small Livestock Experiment Station (1984-1991), the Faculty of Agriculture at Shizuoka University (1987-1988), and as Representative Director of the Shizuoka City Emergency Animal Hospital (2015-2020). He currently serves the Director of the Sugiyama Veterinary Clinic, and holds numerous parallel posts, including committee member for the Japan Veterinary Medical Association, Vice President of the Shizuoka Animal Welfare Association, Vice President of the Japanese Clinical Society of Rabies, as well as a cooperative researcher at Azabu University.
Toshihiro Tanaka (Head, Department of Pediatrics, Shizuoka Kosei Hospital)
 Born in Aoi-ku, Shizuoka City, Dr. Tanaka graduated from the University of Tsukuba’s School of Medicine in March 1992. After training and practicing at hospitals within and outside Shizuoka Prefecture, and studying abroad at the Division of Clinical Pharmacology at The Hospital for Sick Children in Toronto, Canada, he has been serving as the Head of the Department of Pediatrics at Shizuoka Kosei Hospital since April 2010. His fields of interest include vaccination, pediatric infectious diseases, clinical pharmacology, intestinal bacteria, and breastfeeding. He is a member of numerous academic societies, including the Japan Pediatric Society, the Japanese Society for Pediatric Infectious Diseases (Board Member, Chair of Pharmaceutical Affairs Committee), the Japanese Association for Infectious Diseases, the Japanese Society for Vaccinology (Board Member), and many others.
Born in Aoi-ku, Shizuoka City, Dr. Tanaka graduated from the University of Tsukuba’s School of Medicine in March 1992. After training and practicing at hospitals within and outside Shizuoka Prefecture, and studying abroad at the Division of Clinical Pharmacology at The Hospital for Sick Children in Toronto, Canada, he has been serving as the Head of the Department of Pediatrics at Shizuoka Kosei Hospital since April 2010. His fields of interest include vaccination, pediatric infectious diseases, clinical pharmacology, intestinal bacteria, and breastfeeding. He is a member of numerous academic societies, including the Japan Pediatric Society, the Japanese Society for Pediatric Infectious Diseases (Board Member, Chair of Pharmaceutical Affairs Committee), the Japanese Association for Infectious Diseases, the Japanese Society for Vaccinology (Board Member), and many others.
Takahiro Mochizuki (Department of Pharmacy, Shizuoka Cancer Center)
 Mr. Mochizuki received his Master’s degree from the Graduate School of Pharmaceutical Sciences at Hokkaido University in 2004 and joined the Shizuoka Cancer Center in the same year. As a specialized pharmacist, he contributes to improving the quality and safety of pharmacotherapy in cancer treatment. He serves as a council member for the Japanese Society of Chemotherapy and the Japanese Society for Infection Prevention and Control. He is a board-certified infection control pharmacist and antimicrobial chemotherapy pharmacist, dedicated to infection control and appropriate drug therapy for cancer patients.
Mr. Mochizuki received his Master’s degree from the Graduate School of Pharmaceutical Sciences at Hokkaido University in 2004 and joined the Shizuoka Cancer Center in the same year. As a specialized pharmacist, he contributes to improving the quality and safety of pharmacotherapy in cancer treatment. He serves as a council member for the Japanese Society of Chemotherapy and the Japanese Society for Infection Prevention and Control. He is a board-certified infection control pharmacist and antimicrobial chemotherapy pharmacist, dedicated to infection control and appropriate drug therapy for cancer patients.

*A report on the seminar has been published. (December 9, 2025)
Health and Global Policy Institute (HGPI) hosted a special seminar titled “Rising to New Challenges in Health Sciences for Future Society: Coming Novel Developments in the Field of Epilepsy in Japan and Globally”.
Focusing on epilepsy, a neurological disorder affecting approximately 50 million people worldwide, the seminar brought together people living with epilepsy, experts, and policymakers to discuss the latest developments in epilepsy treatment and explore potential solution for addressing related challenges in the future.
Although epilepsy is currently one of the most common neurological disorders, such as challenges remain in terms of diagnosis and limited access to appropriate treatment. Furthermore, in many countries, such as social stigma and a lack of information hinder patients from accessing the care they need, resulting in a serious issue known as the “treatment gap.”
While notable efforts are being made both in Japan and around the world to address this issue, people living with epilepsy continue to face a range of socio-economic challenges beyond their physical health, such as psychological impacts, limitations in daily life, and restricted employment opportunities associated with the condition.
This seminar was grounded on the voices of people with lived experience, while incorporating insight from experts and policymakers, to create a discussion -focused forum on the future of neurological disorder treatment. Through this, we aimed to deepen public understanding of epilepsy and other neurological disorders and contribute to the development of better treatment.
[Event Overview ]
- Date & Time: Thursday, September 18, 2025; 13:00-15:00 JST
- Format: In-person event with online streaming (Simultaneous interpretation will be provided)
- Venue: Belgium Pavilion, World Expo 2025 Osaka, Kansai
- Language: Japanese / English (English available for online streaming)
- Host: Health and Global Policy Institute (HGPI)
- Sponsors: UCB Japan Co. Ltd., LivaNova Japan K. K.
- Cooperation: Belgian Commission General for International Exhibitions
[Program] (Titles omitted, no particular order)
| 13:00-13:05 | Explanatory introduction and Greetings from Hosts |
| 13:05-13:35 | Keynote Lecture “Considering the Past and Future of Epilepsy Treatment from a Global Perspective” |
| Kensuke Kawai (Professor & Director, Department of Neurosurgery, Jichi Medical University/ President, The Japan Epilepsy Society) | |
| 13:40-14:40 | Panel Discussion “Issues and Solutions for Epilepsy Treatment from the Perspectives of People Living with Epilepsy” |
|
Panelists Moderator |
|
| 14:40-15:00 | Q&A |

<POINTS>
- Plastic pollution is no longer just an environmental issue but a significant global health security concern. Hazardous chemicals from plastics have been linked to various health problems, and the discovery of microplastics in human bodies continues to pose unknown risks.
- Since 2022, the path to a Global Plastics Treaty has been fraught with challenges, marked by fundamental disagreements between nations advocating for ambitious, health-protective regulations (including production caps) and those prioritizing waste management and economic development.
- The conclusion of the INC-5.2 in Geneva, Switzerland could not reach a final agreement on the treaty due to significant disagreements on core issues such as production, specific plastic products, and funding mechanisms, necessitating further rounds of negotiations to be held at a later date.
- Domestically, Japan’s initiatives focus on a comprehensive lifecycle approach to plastics, emphasizing resource circulation. In addition, Japan has been active in monitoring and data collection globally (particularly in ocean microplastics), presenting an opportunity for Japan to lead with innovative solutions grounded on evidence.
Introduction
Since its commercial introduction in the mid-20th century, plastic has transformed nearly every aspect of modern life, from medicine and engineering to everyday consumer goods. However, this transformation has come at a cost: the escalating plastic pollution now poses significant threats to both environmental and public health, making it one of the most pressing challenges in contemporary environmental policy. The conclusion of the second part of the fifth session of the Intergovernmental Negotiating Committee (INC-5.2) in Geneva, Switzerland, underscored both the urgency and complexity of addressing this global challenge. Despite intensive negotiations, securing a comprehensive Global Plastics Treaty remains elusive, representing a critical test for international environmental diplomacy and multilateral cooperation. This policy column analyzes the complex international negotiating process, examines Japan’s evolving position and contributions to these discussions, and explores how global developments intersect with domestic plastic policy initiatives.
Plastic Pollution as a Health Security Issue
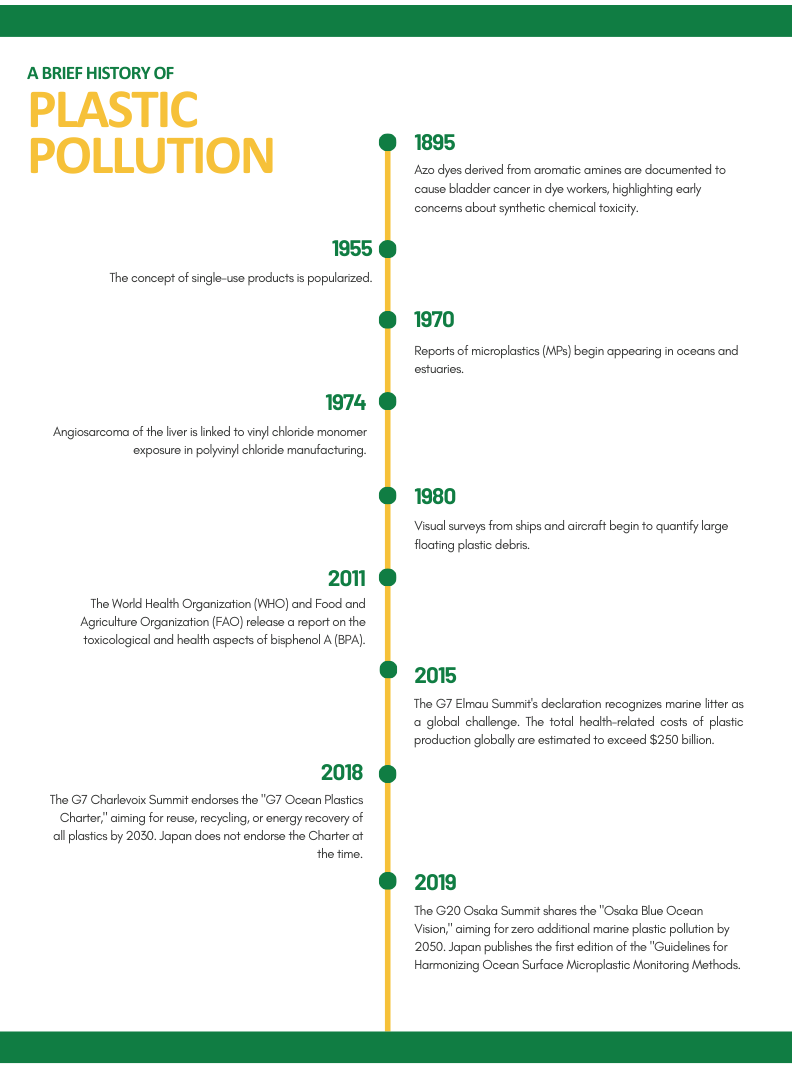
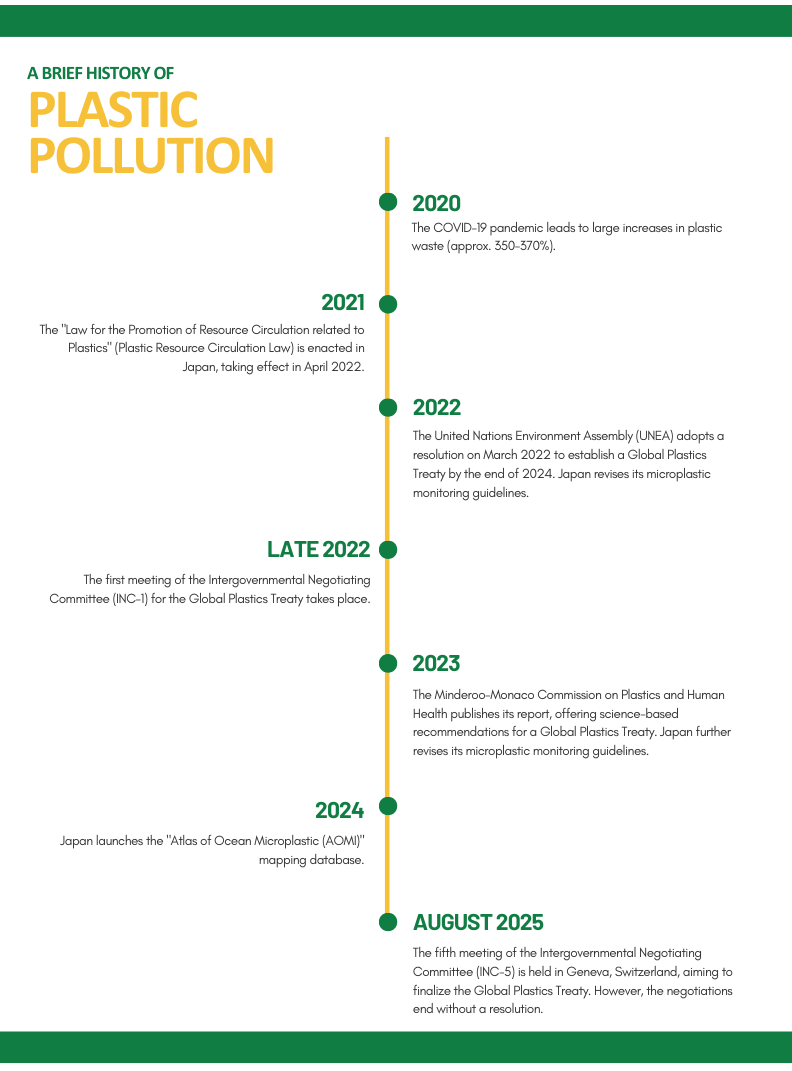
Figure 1: A brief history of plastic pollution
The recognition of plastic pollution as a global health security issue reflects an acknowledgement of the deep connections between ecological damage and human wellbeing. Current projections indicate that without decisive interventions, plastic waste entering water systems could surge from 23 million to 37 million tons annually by 2040, fundamentally changing the relationship between humans and their environment. Recent findings published by the Minderoo-Monaco Commission in 2023 highlighted that plastics harm both human and planetary health, from heightened risk of childhood cancer brought about by early exposure to plastics, to the discovery of microplastic and nanoplastic particles (MNPs) in marine species, including species consumed by humans. This trajectory raises concerns regarding large-scale introductions of new chemical compounds with poorly understood long term-effects on human health.
Scientific evidence supporting this concern has grown in recent years. The dangers of plastics to human health were first recognized as early as the 1970s, through four cases of hepatic angiosarcoma among polyvinyl chloride (PVC) polymerization workers in Kentucky, USA. Since then, research has identified over 16,000 chemicals used in plastic production processes, with at least 4,200 classified as “highly hazardous” to human health and environmental systems, yet only 6% are currently regulated by international treaties. Food contact materials such as tableware, food containers, drinking water bottles, sachets, and food processing equipment can all release chemicals, which then enter the human body through ingestion, inhalation, and dermal absorption.
The health implications are serious, with peer-reviewed studies establishing clear links between plastic-related chemicals and various health problems, including cancers, genetic mutations, reproductive system damage, neurological dysfunction, and weakened immune systems. The discovery of microplastics in human blood and breastmilk underscores the urgency of developing comprehensive policies. From a health economics perspective, the costs of regulatory inaction on this chemical and plastic pollution crisis are projected to reach 10% of global GDP, with health-related damages alone estimated at hundreds of billions of dollars annually.
In response to this, the United Nations Environment Assembly (UNEA-5.2) adopted a historic resolution in March 2022 to develop an international legally binding instrument on plastic pollution by the end of 2024, taking a comprehensive approach to the entire lifecycle of plastics. However, the path to a robust treaty has not been easy. Negotiations at INC-1 (Uruguay), INC-2 (Paris), INC-3 (Nairobi), INC-4 (Ottawa), and INC-5.1 (Busan) have largely been divisive.

Figure 2: Overview of International Negotiating Committee (INC) negotiations
International Environmental Law Negotiations and Health Integration
At the current pace of plastic production, recycling alone fails to eradicate the problem, as only less than 10% of all plastic waste is currently recycled worldwide, necessitating a full life-cycle approach to the plastic crisis. International efforts to regulate plastic have been shaped by competing approaches between market-focused and health-first approaches. The negotiating process at the Global Plastics Treaty discussions has also revealed fundamental disagreements about the scope and intensity of international regulation.
Over 100 nations have advocated for plastic production caps and strict chemical regulation based on precautionary principles. Their emphasis on a full-lifecycle approach reflects growing recognition that effective health protection requires intervention at all stages of plastic production, distribution, use, and disposal. In contrast, major petrochemical-producing states, including Saudi Arabia, the United States, Russia, and China, have favored regulatory frameworks that prioritize waste management over production restrictions, viewing plastics as essential to economic development. Notably, some negotiations have seen proposals to remove treaty sections addressing supply chains or health considerations entirely, indicating the depth of disagreement over how broad regulations should be.
Financial mechanisms represent another critical part of the negotiations, with developing countries emphasizing that treaty implementation requires “adequate, accessible, new, and additional financial resources.” Some countries have proposed compensation mechanisms for pollution-related damages, reflecting broader debates about environmental justice and shared responsibilities. Financing schemes have been suggested, such as the Polymer Premium, which could help bridge the fiscal gap especially for developing countries. These discussions are closely linked to health considerations, as developing countries often experience disproportionate health burdens from plastic pollution while having limited ability to regulate it.
Despite high hopes, the fifth session of the Intergovernmental Negotiating Committee’s resumed meeting (INC 5.2) held from August 5 to 15, 2025, concluded without reaching a substantive agreement on the Global Plastics Treaty. Despite intensive negotiations across four working groups, significant differences of opinion remained on key articles, including those concerning production, plastic products (Article 4), and finance (Article 10), as well as the Conference of the Parties (Article 18). While progress was made on other articles such as the objective, product design, releases and leakages, waste management, existing plastic pollution, just transition, and implementation and compliance, the negotiations will need to continue in future resumed sessions. Japan actively participated in the meeting, emphasizing the importance of promoting a full lifecycle approach, clear common standards for plastic products, environmentally sound product design, proper waste management (including Extended Producer Responsibility), national action plans, and resource mobilization from all funding sources.
Japan’s Domestic Policy Evolution
Japan’s domestic policy evolution (particularly on ocean plastics) is closely linked to international frameworks. Notably, the G20 Action Plan on Marine Litter, built on the Osaka Blue Ocean Vision which aims to reduce marine plastic litter to zero by 2050, provides a voluntary platform for sharing national policies promoting circular economy initiatives. Complementing this, the G20 Implementation Framework for Actions on Marine Plastic Litter was created to support the practical implementation of the Action Plan. Local initiatives across Japanese prefectures and municipalities also demonstrate Japan’s multi-level approach, ranging from marine litter management systems in Okayama City to symposia on recycling technologies in Tokyo.
The institutional framework supporting Japan’s domestic plastic governance includes amendments to the Law for the Act on Promoting the Treatment of Marine Debris (2018) and the development of a Plastic Resource Circulation Strategy (2019) that emphasizes reduction of single-use plastics, promotion of reuse and recycling, and energy recovery from used plastics. This strategy laid the foundation for later legal actions such as the “Act on Promotion of Resource Circulation for Plastics”, which came to force in April 2022. The act aims to promote the efficient use and conservation of resources and reduce plastic waste throughout the entire lifecycle of plastic products, from design to disposal. The law is based on the fundamental principle of “3R + Renewable,” which stands for Reduce, Reuse, Recycle, and shifting to renewable resources.
Specifically, the law requires businesses to consider resource circulation from the product design stage, including reducing plastic usage, promoting reuse, and incorporating recycled materials. For certain designated categories of single-use plastic products, businesses that provide them are obligated to take measures to reduce and rationalize their use, with specific requirements applying when their efforts are judged insufficient. In addition, companies that generate large volumes of industrial plastic waste must take steps to reduce waste, separate it properly, and promote recycling. Through this framework, the government, local authorities, businesses, and consumers are expected to cooperate in curbing plastic waste by reducing reliance on single-use plastics and enhancing recycling, with the ultimate goal of realizing a circular economy and reducing environmental impacts.
Japan has also been at the forefront of ocean microplastic research. In 2019, Japan published the first edition of its “Guidelines for Harmonizing Ocean Surface Microplastic Monitoring Methods”. These guidelines underwent further revisions in both 2022 and 2023 to incorporate new findings and methodological improvements. Building on this foundation, Japan launched the “Atlas of Ocean Microplastic (AOMI)” mapping database in May 2024, creating a comprehensive resource for tracking microplastic distribution across ocean surfaces.
For a sustainable future, Japan’s plastic policies must continue to evolve. Collaboration among individuals, businesses, and government to shift society from a “disposable” mindset to a “circular” one will be key to preserving the environment.
Economic Benefits of a Global Plastics Treaty
Recent economic analysis commissioned by the Business Coalition for a Global Plastics Treaty, for which WWF Japan serves as the secretariat, provides strong evidence for harmonized regulations regarding plastic pollution. The study shows that implementing international rules for phaseouts/eliminations (Article 3), product design (Article 5), and waste management/EPR (Article 8) would yield significant economic benefits for Japan and other countries adopting similar approaches. For Japan specifically, the analysis indicates the following benefits under global regulations compared to fragmented national approaches by 2040:
- Recycled material production could increase by 90%
- Waste management costs could be reduced by 10% from 2026 to 2040
- International coordination would achieve a 2.25-fold greater reduction in problematic single-use plastics
- Economic activity in the regional plastics value chain (including Japan, South Korea, Australia, and New Zealand) is projected to increase by 7%
- Employment in the regional plastics value chain (including Japan, South Korea, Australia, and New Zealand) is projected to increase by 5%
These findings suggest that comprehensive international regulation supports both national economic interests and environmental and health protection goals, further indicating that fragmented approaches may impose higher costs on domestic industries while providing fewer health and environmental benefits.
Conclusion
The inconclusive outcome of INC-5.2 in Geneva underscores the persistent challenges facing international environmental diplomacy in addressing complex issues such as plastic pollution. However, Japan’s active participation and comprehensive domestic policy framework position it to demonstrate leadership in pioneering health-protective solutions that align with economic interests. There is compelling evidence that comprehensive international regulation can advance both health protection objectives and national economic interests.
As negotiations continue in future resumed sessions, the trajectory of global plastic governance will significantly influence not only international environmental law but also the broader development of health-centered approaches to 21st-century environmental challenges. The ultimate success of a Global Plastics Treaty will depend on bridging the divide between these approaches, recognizing that the health and economic costs of regulatory inaction far exceed the investments required for comprehensive intervention across the plastic lifecycle.
References
- Business Coalition for a Global Plastics Treaty. (2025). The economic rationale for a Global Plastics Treaty underpinned by mandatory harmonised regulation — A modelling exercise (June 2025). Ellen MacArthur Foundation. Retrieved July 3, 2025, from https://content.ellenmacarthurfoundation.org/m/5464570e082d536b/original/Business-Coalition-Economic-Rationale-Modelling-Doc.pdf
- Falk, H. (1987). Vinyl chloride-induced hepatic angiosarcoma. Princess Takamatsu Symposium, 18, 39–46. Retrieved July 3, 2025, from https://pubmed.ncbi.nlm.nih.gov/3506545/
- G20 Marine Plastic Litter. (2024). Towards Osaka Blue Ocean Vision: G20 implementation framework for actions on marine plastic litter. https://g20mpl.org/
- Global Plastic Laws. (n.d.). UN plastics treaty. Retrieved July 3, 2025, from https://www.globalplasticlaws.org/un-global-plastics-treaty
- Government of Japan. (2024, November 25). Japan national statement under agenda item 4, INC-5: The fifth session of Intergovernmental Negotiating Committee to develop an international legally binding instrument on plastic pollution, including in the marine environment [PDF]. United Nations Environment Programme. Retrieved July 3, 2025, from https://resolutions.unep.org/incres/uploads/japan_national_statement_under_agenda_4_inc5.pdf
- Health Policy Watch. (2025, April 17). The health crisis that could make or break the UN plastics treaty. Retrieved July 3, 2025, from https://healthpolicy-watch.news/the-health-crisis-that-could-make-or-break-the-un-plastics-treaty/
- ICLEI Japan. (n.d.). Call for participation in the Global Plastic Treaty to reduce plastic use. Retrieved July 3, 2025, from https://japan.iclei.org/en/news/call-for-participation-in-the-global-plastic-treaty/
- Intergovernmental Negotiating Committee. (2025, February 10). Draft report of the Intergovernmental Negotiating Committee to develop an international legally binding instrument on plastic pollution, including in the marine environment, on the work of the first part of its fifth session (UNEP/PP/INC.5/8) [PDF]. United Nations Environment Programme. Retrieved July 3, 2025, from https://wedocs.unep.org/bitstream/handle/20.500.11822/47162/INC_5_1_Report.pdf
- Kyodo News. (2024, June 3). Over 70 nations to call for international plastic pollution reduction targets. Kyodo News. Retrieved July 3, 2025, from https://english.kyodonews.net/articles/-/54762?phrase=Toshiba+&words=
- Landrigan, P. J., Dunlop, S., Treskova, M., Raps, H., Symeonides, C., Muncke, J., et al. (2025). The Lancet Countdown on health and plastics. The Lancet. Advance online publication. https://doi.org/10.1016/S0140-6736(25)01447-3
- Landrigan, P. J., Raps, H., Martins, D., et al. (2023). The Minderoo-Monaco Commission on Plastics and Human Health. Annals of Global Health, 89(1), Article e1. https://doi.org/10.5334/aogh.4056
- Michida, Y., et al. (2019). Guidelines for harmonizing ocean surface microplastic monitoring methods. Ministry of the Environment Japan.
- Minderoo Foundation. (2024). The polymer premium: A fee on plastic pollution. Retrieved July 3, 2025, from https://cdn.minderoo.org/content/uploads/2024/04/21232940/The-Polymer-Premium-a-Fee-on-Plastic-Pollution.pdf
- Ministry of the Environment. (2009). Act on promoting proper treatment of coastal drift debris. e-Gov Law Search. Retrieved July 3, 2025, from https://laws.e-gov.go.jp/law/421AC1000000082
- Ministry of the Environment. (2019). Plastic resource circulation strategy. Retrieved July 3, 2025, from https://plastic-circulation.env.go.jp/about/senryaku
- Ministry of the Environment. (2024). Summary of outcomes of the fifth session of the Intergovernmental Negotiating Committee for the development of an international legally binding instrument (treaty) on plastic pollution. Retrieved July 3, 2025, from https://www.env.go.jp/press/press_04058.html
- Ministry of the Environment, Government of Japan. (2025, August 5). Summary of the fifth resumed session of the Intergovernmental Negotiating Committee for a legally binding international agreement on plastic pollution. Retrieved September 10, 2025, from https://www.env.go.jp/press/press_00461.html
- Ministry of the Environment, Japan. (2024, May 8). Release of the marine plastic litter mapping database “Atlas of Ocean Microplastics (AOMI).” Retrieved July 3, 2025, from https://www.env.go.jp/en/press/press_02788.html
- Ministry of the Environment, Japan. (n.d.). Atlas of Ocean Microplastics (AOMI). Retrieved August 22, 2025, from https://aomi.env.go.jp/
- Okayama City. (2023, June 19). Marine Litter Gatekeeper. Retrieved July 9, 2025, from https://www.city.okayama.jp/harmonia/0000049028.html
- Rever Co., Ltd. (2023, February 9). Understanding the Plastic Resource Circulation Promotion Act in 10 minutes: The act and the wide-area certification system. Ecoo Online. Retrieved July 3, 2025, from https://www.re-ver.co.jp/ecoo-online/waste-disposal-low/20220208.html
- The Japan Times. (2024, November 29). Showdown looms on plastic treaty days before deadline. The Japan Times. Retrieved July 3, 2025, from https://www.japantimes.co.jp/environment/2024/11/29/plastics-treaty-showdown/
- Tokyo Metropolitan Government. (2023, April 4). Online symposium: The future of plastic recycling – Advanced technologies for closed-loop recycling [Video]. YouTube. Retrieved July 3, 2025, from https://www.youtube.com/watch?v=U_rLm4IkWlg
- United Nations Environment Programme. (2025). Chair’s revised text proposal – 15 August 2025 as at 00:48. Retrieved September 10, 2025, from https://resolutions.unep.org/incres/uploads/chairs_revised_draft_text_proposal_-_15.08.25_at_00.482.pdf
- WWF Japan. (2025, June 27). New analysis released ahead of final negotiations on the international plastics treaty: Legally binding, harmonized rules benefit economic activities—Plastic-related economic activities projected to increase by 31% globally. Retrieved July 3, 2025, from https://www.wwf.or.jp/press/5993.html
- Wheeler, J. B., & Solomon, H. (1974). Angiosarcoma of liver in the manufacture of polyvinyl chloride. Journal of Occupational Medicine, 16(3), 150–151. Retrieved July 3, 2025, from https://doi.org/10.1097/00043764-197403000-00005
- Yamamoto MRC. (2025). What is the Plastic Resource Circulation Promotion Act? Overview and explanation of the 12 targeted items. Retrieved July 3, 2025, from https://www.yamamoto-mrc.co.jp/column/industrial/1526/
- Zimmermann, L., Scheringer, M., Geueke, B., et al. (2022). Implementing the EU chemicals strategy for sustainability: The case of food contact chemicals of concern. Journal of Hazardous Materials, 437, 129167. Retrieved July 3, 2025, from https://doi.org/10.1016/j.jhazmat.2022.129167
Authors
Gail Co (Program Specialist, Health and Global Policy Institute)
Joji Sugawara (Vice President, Health and Global Policy Institute)